Home » Coding Services Companies
HCC Coding Solutions & AI-Powered Services for Medical Coding Companies
Achieve Accurate Medical Coding Compliance While Meeting Tight Deadlines
Tailored HCC Coding Solutions for Medical Coding Companies
Many healthcare providers and physicians may not provide detailed documentation or may use ambiguous language when describing medical conditions, making it challenging for coders to assign accurate HCC codes. Additionally, Hierarchical Condition Category (HCC) coding requires a high level of specificity due to varying severity levels, adding complexity as coders must stay updated with the latest CMS codes and regulations.
Given the critical role of accurate medical coding in insurance reimbursements and financial aspects of patient care, medical coding and billing companies must ensure their teams are well-versed in these complexities to maintain compliance and deliver high-quality services.
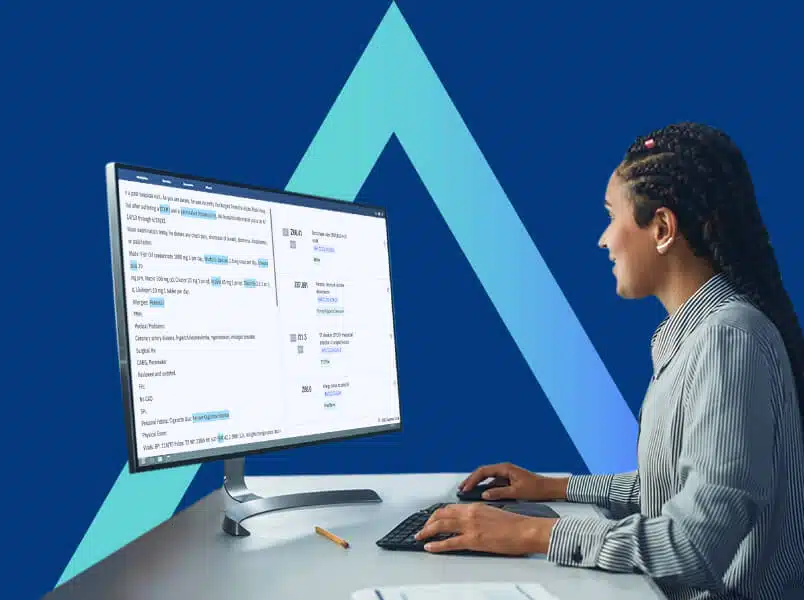
Metacare AI’s advanced HCC coding solutions empower in-house medical coders to enhance compliance, streamline patient data review, and optimize the chart audit process. Additionally, our expert HCC coding services help organizations meet tight project deadlines efficiently while ensuring accuracy and regulatory adherence.
Advanced Risk Adjustment Technologies for Value-Based Care Organizations
HCC CAPTURE
Chart Review for Precision Risk Adjustment
Optimize risk adjustment workflows and minimize errors with Metacare AI’s advanced solutions, ensuring faster turnaround times and superior coding accuracy.

HCC COMPASS
Chart Audit Technology for Accurate HCC Coding
Leverage advanced AI-powered audit solutions to automatically detect HCC coding discrepancies or missing data, ensuring accuracy and compliance in billing claims processing.
Maximize the Benefits of Metacare AI's Risk Adjustment Technology.
Our Comprehensive Risk Adjustment Solutions for Medical Coding Companies

HCC Coding
Enhance HCC coding efficiency while minimizing overhead costs associated with staffing and technology investments.
Chart Review
Optimize time and resources by eliminating the need for extensive staff training and management in complex HCC coding tasks.

Chart Audit
Maintain quality assurance and regulatory compliance while minimizing costs linked to in-house medical coding staff.
Risk Adjustment Insights for Medical Coding Companies
Why Choose Metacare AI’s Customized HCC Coding Technology Solutions & Services for Medical Coding Companies
NLP
This technology enables HCC coders to interpret complex medical terminology with greater speed and accuracy, enhancing efficiency like never before.

Knowledge Graph
Knowledge graphs enhance accuracy in patient diagnosis coding by minimizing errors and ensuring precise HCC code mapping.
OCR
Efficiently process large volumes of data with AI-driven automation, eliminating time-consuming manual entry and reducing errors in HCC coding.

ML/DL AI
Optimize coding capacity and efficiency with AI-powered solutions, ensuring accurate HCC coding that accurately reflects patient condition severity.
API
APIs enable secure data exchange across healthcare systems while ensuring patient privacy and maintaining strict confidentiality standards.
How We Support Your Healthcare Organization
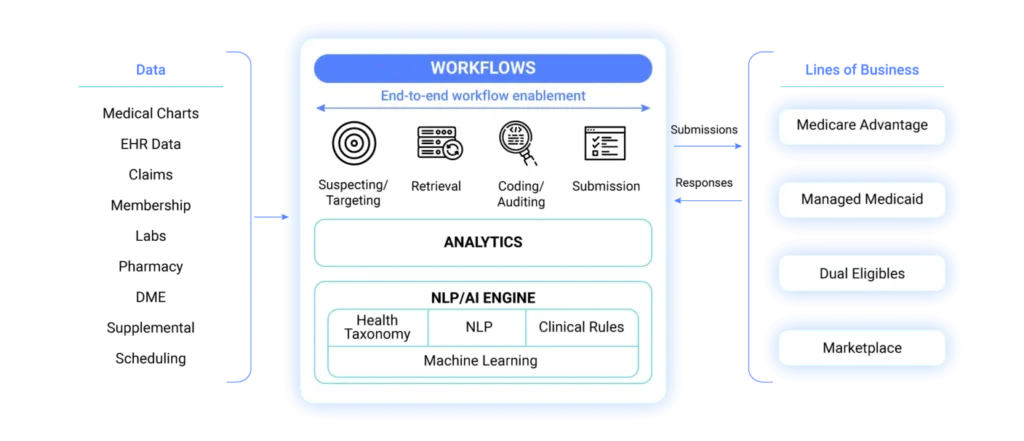

The World's First AI-Driven Personalized Risk Adjustment Coding & Audit Platform
Client Testimonials
FAQs related to health plans
Keeping up with HCC coding reviews and audits can be a complex and resource-intensive process.
Outsourcing these tasks offers significant advantages for medical coding and billing companies. It enables them to focus on core operations while leveraging expert-driven HCC coding reviews and audits. Additionally, outsourcing provides access to specialized AI-powered technology and certified coding professionals that may not be available in-house.
Another key benefit is enhanced compliance with CMS regulations. Accurate HCC coding reviews and audits are essential for determining Risk Adjustment Factor (RAF) scores, which directly impact Medicare Advantage reimbursements. Non-compliance with CMS guidelines can lead to financial penalties or exclusion from Medicare Advantage programs.
By outsourcing HCC coding reviews and audits, medical coding and billing companies can improve efficiency, minimize coding errors, ensure regulatory compliance, and enhance overall revenue cycle management, leading to better patient care and optimized financial outcomes.
Medical coding and billing companies have a lot on their plate when it comes to managing the financial side of healthcare. With so many regulations and guidelines to follow, it’s no wonder that outsourcing medical coding and billing review and audit tasks has become such a popular option. But what should these companies look for in an outsourced partner?
Firstly, experience is key. The chosen partner should have a proven track record of success in the industry, with knowledgeable staff who are up-to-date on all relevant regulations. They should also provide clear communication channels between themselves and the medical coding and billing company, ensuring that any questions or concerns can be addressed quickly.
Accuracy is another important factor – errors could lead to costly audits or even legal issues down the line. Therefore, the outsourcing partner must demonstrate a rigorous quality control process.
Finally, flexibility is crucial as different clients will have different needs; there cannot be a one-size-fits-all approach when it comes to reviewing medical codes and bills.
By finding an experienced partner that prioritizes accuracy while remaining flexible in its approach to each client’s unique needs, medical coding, and billing companies can ensure they stay compliant with industry standards while providing top-notch services to clients.
With advanced NLP technology, medical coding and billing companies can optimize workflows, enhance coding accuracy, minimize claim denials and rejections, and ensure compliance with regulatory standards. By leveraging AI-driven audits and targeted reviews focused on high-risk areas or evolving healthcare policies, NLP solutions provide deeper insights into complex medical data. This not only improves operational efficiency but also maximizes reimbursement potential and profitability. Implementing a robust NLP-powered platform enables seamless healthcare data management, ensuring precision and compliance in risk adjustment coding.
Medical coding and billing companies in the U.S. face increasing challenges in maintaining accuracy and efficiency amid rising demands. Metacare AI’s deep learning technology provides a powerful solution to streamline operations and optimize medical coding processes for healthcare providers.
By leveraging advanced deep learning algorithms, medical coding and billing companies can automate key tasks such as identifying diagnosis codes, detecting errors, and ensuring accurate claims processing. This automation not only enhances efficiency but also minimizes errors, leading to faster reimbursements and improved revenue cycle management.
Additionally, deep learning technology helps uncover patterns in claims data, identifying potential fraud or billing inconsistencies. By analyzing vast datasets, AI-driven insights can flag anomalies for review, ensuring compliance with regulatory standards and reducing financial risks.
Medical coding and billing companies in the U.S. face complex challenges that demand efficient solutions. Metacare AI’s machine learning technology streamlines operations by automating key processes such as claim submissions, patient information verification, and insurance eligibility checks, reducing manual effort and errors.
With advanced AI-driven algorithms, medical coders can enhance accuracy by analyzing vast datasets from electronic health records (EHRs), enabling faster and more precise code selection. Additionally, machine learning strengthens fraud detection by identifying suspicious trends in claims data, reducing financial risks.

